Para-aortic lymphadenectomy in endometrial cancer
Lancet, Volume 376, Issue 9740, Pages 511 - 512, 14 August 2010 <Previous Article|Next Article>doi:10.1016/S0140-6736(10)61245-7Cite or Link Using DOI
Clare Griffin a, Ann Marie Swart a, Wendi Qian a, Henry Kitchener b
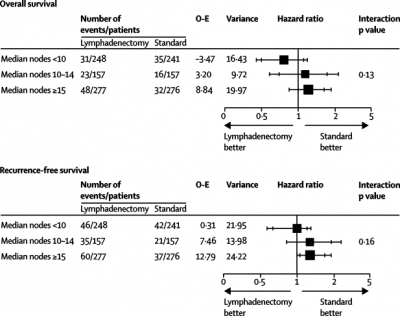
We were not surprised that the results of the retrospective cohort analysis of SEPAL1 differed from those of two randomised controlled trials.2, 3 With a hazard ratio for overall survival of 1·16 (favouring no lymphadenectomy) in ASTEC,2 it is extremely unlikely that conclusions would change with long-term follow-up because there would have to be a large, late effect which is not suggested by SEPAL. Lymphadenectomy significantly increases moderate and severe morbidity, particularly lymphoedema, and removing more lymph nodes might not be better (figure).
ASTEC effect of lymphadenectomy in centres grouped according to median nodes removed
O-E=observed minus expected. Outer bars show 99% CI, inner bars show 95% CI.
Lack of information about methods makes the results impossible to interpret, particularly patient selection and surgery details (operation length, blood loss, postoperative hospital stay, and related deaths). The median age of 56 years suggests substantial selection (median age was 63 years in ASTEC). Data were gathered over 18 years and information about the distribution of patients in each group across time and any time effect on survival is important. Bias due to differences between the hospitals cannot be excluded, with differing adjuvant protocols and almost double the number of pelvic nodes removed in some hospitals compared with others.
In women at intermediate or high risk of recurrence, the substantial difference in adjuvant chemotherapy received (77% vs 45%) is important. Chemotherapy reduces distal metastases,4 potentially improving survival and the effect of para-aortic lymphadenectomy. The benefit in high-risk patients receiving chemotherapy is only just significant. Since type of lymphadenectomy and adjuvant treatment were independent risk factors for overall survival, there are strong statistical arguments for sensitivity analyses excluding those receiving adjuvant treatment.
Aortic lymphadenectomy was not assessed in either randomised trial and the results of this observational study do not invalidate the conclusions of these trials nor provide conclusive evidence of a real treatment effect.
We declare that we have no conflicts of interest.
References
1 Todo Y, Kato H, Kaneuchi M, Watari H, Takeda M, Sakuragi N. Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL study): a retrospective cohort analysis. Lancet 2010; 375: 1165-1172. Summary | Full Text | PDF(273KB) | CrossRef | PubMed
2 The writing committee on behalf of the ASTEC study group. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet 2009; 373: 125-136. Summary | Full Text | PDF(250KB) | CrossRef | PubMed
3 Panici PB, Basile S, Maneschi F, et al. Systematic pelvic lymphadenectomy vs no lymphadenectomy in early-stage endometrial cancer: randomized clinical trial. J Natl Cancer Inst 2008; 100: 1707-1716. CrossRef | PubMed
4 Maggi R, Lissoni A, Spina F, et al. Adjuvant chemotherapy vs radiotherapy in high-risk endometrial carcinoma: results of a randomised trial. Br J Cancer 2006; 95: 266-271. CrossRef | PubMed
a Cancer Group, MRC Clinical Trials Unit, London NW1 2DA, UK
b University of Manchester, Manchester, UK